Hydrocephalus in Adults
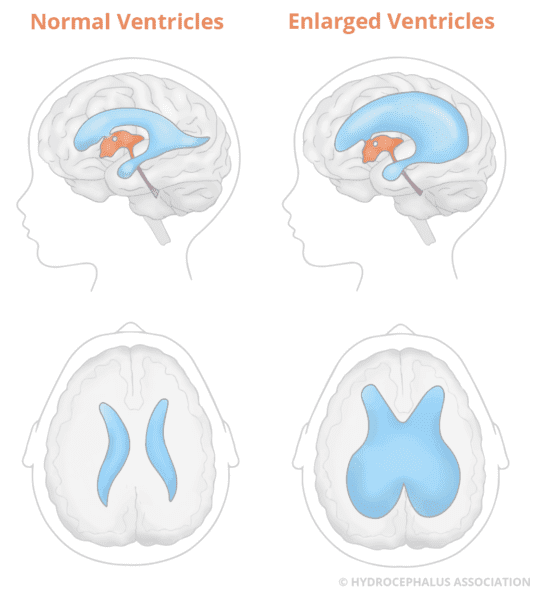
Hydrocephalus occurs when there is a buildup of fluid, known as cerebrospinal fluid (CSF), in cavities called ventricles inside the brain.
Anyone at any age can be diagnosed with hydrocephalus. Hydrocephalus in young and middle-aged adults is a unique and often confusing condition, as it is vastly different from hydrocephalus diagnosed in infancy and childhood and normal pressure hydrocephalus (NPH) (typically found in adults aged 60 or over). Hydrocephalus in this age group presents a host of challenges that go far beyond routine or specialized medical care as it encompasses psychosocial, emotional, and occupational issues as well.
For more detailed information on hydrocephalus, visit About Hydrocephalus and Cerebrospinal Fluid Dynamics Relevant to Hydrocephalus.
What are the Types and Causes of Hydrocephalus in Adults?
There are four categories of adults living with hydrocephalus:
1. Adults newly diagnosed with congenital hydrocephalus
Hydrocephalus present at birth is referred to as congenital hydrocephalus, and while you may be hearing of this diagnosis as an adult for the first time, many discover that they have had this condition their entire life.
It is unclear as to why hydrocephalus can remain dormant for years, as some people don’t notice symptoms until adolescence or even adulthood. At times, asymptomatic hydrocephalus is identified on CT or MRI of the brain that was obtained for completely unrelated neurologic symptoms, such as mild head trauma caused by an unrelated injury. Likewise, many patients undergo brain imaging for headaches or dizziness when such symptoms are caused by unrelated problems such as migraines or inner ear disorders. In both examples, hydrocephalus may have been identified had the scan been performed before the onset of the trauma or symptoms.
With undiagnosed hydrocephalus, either the fluid slowly builds up to a point where it affects the brain’s normal function or the fluid spaces (ventricles) in the brain can slowly become larger over time. This causes a subtle ongoing injury that gradually weakens the brain’s ability to compensate. Such cases are sometimes classified as decompensated congenital hydrocephalus.
Congenital hydrocephalus is caused by a complex interaction of genetic and environmental factors during fetal development. The most common causes of congenital hydrocephalus are:
-
- Spina bifida
- Aqueductal stenosis
- Brain malformations
To learn more, visit Congenital Hydrocephalus.
2. Adults who acquire hydrocephalus
Acquired hydrocephalus is the form of hydrocephalus that develops any time after birth.
Both children and adults can be diagnosed with acquired hydrocephalus. The most common causes are:
-
- Head injuries
- Brain tumors
- Intraventricular hemorrhage (brain bleed)
- Meningitis or other infection of the brain or spinal cord
To learn more, visit Acquired Hydrocephalus.
3. Adults who are diagnosed and treated in childhood (transitioning(ed) adults)
Investments in research and advances in technology, as well as diagnostic and treatment protocols, are helping more and more children with hydrocephalus to grow up and transition into adulthood and adult medical care, leading full and active lives.
We’re here to assist you every step of the way as you navigate this important phase in your healthcare journey.
4. Adults diagnosed over the age of 60
Normal pressure hydrocephalus (NPH) occurs in older adults, and this is typically diagnosed in individuals 60 and older.
Normal pressure hydrocephalus (NPH) is an accumulation of cerebrospinal fluid (CSF) that causes the ventricles in the brain to become enlarged, but there is little or no increase in the pressure within the ventricles. However, in some NPH patients, CSF pressure does fluctuate from high to normal to low when monitored.
For more information on NPH and the types and causes of NPH visit our page on NPH.
There are other classifications of hydrocephalus that you might hear when talking to your doctor, particularly around the time of diagnosis. These can include:
-
- Compensated or arrested hydrocephalus
- Communicating hydrocephalus
- Non-communicating hydrocephalus, also known as obstructive hydrocephalus
For more detailed information, visit Types and Causes.
What are the Symptoms of Hydrocephalus in Adults?
The symptoms of hydrocephalus in adults are similar in some ways to those of NPH in the elderly but are often much more subtle. Still, they can greatly impact patients’ lives. In severe cases, symptoms might make it difficult to work or handle daily activities.
Symptoms are sometimes disregarded as manifestations of a mid-life crisis or other psychological and emotional issues. As symptoms worsen and the condition goes undiagnosed, one’s ability to function at home and work can be affected, and relationships and employment can be compromised.
Symptoms reported include, but are not limited to:
- Headaches (persistent and/or severe)
- Nausea and vomiting
- Vision problems (double or blurred vision, or difficulty focusing can occur due to increased pressure on the optic nerves)
- Cognitive and memory problems (difficulties with concentration, decision-making, short-term memory issues)
- Balance and coordination issues
- Disturbances in gait (trouble walking)
- Excessive tiredness
- Vertigo (sensation of spinning or dizziness)
- Syncope (fainting)
- Hearing loss
The severity of symptoms and their impact can vary widely among patients, and if symptoms have been present for years, patients may face more pronounced disability. Early diagnosis plays a crucial role in effectively addressing these symptoms.
Nevertheless, as mentioned earlier, because hydrocephalus can be entirely asymptomatic, it is important to recognize that many patients with these symptoms may be suffering from other unrelated neurologic and psychiatric problems. Just detecting hydrocephalus on a brain scan does not “guarantee” that it is a relevant diagnosis and that a shunt is indicated.
How is Hydrocephalus Diagnosed in Adults?
Diagnosing hydrocephalus in adults involves a combination of medical assessments, imaging tests, and evaluations by healthcare professionals. Listed below is an overview of the tests involved.
Brain Imaging Tests
Computed tomography (CT scan) is a reliable procedure for diagnosing and assisting in the management of hydrocephalus. It is a sophisticated technique in which x-ray beams are passed through a patient’s body and pictures of the internal structures, in this case, the brain, are made by the computer.
Unexpected enlargement of the ventricles is often the first clue that hydrocephalus in an adult may be present, but this finding alone is usually not a sufficient reason to proceed to surgical therapy. It is important to remember that hydrocephalus can be compensated (non-progressing) or decompensated (progressing), and further testing is often needed. It is potentially harmful to put a shunt into a person with compensated hydrocephalus, just as it is potentially harmful not to put a shunt into a person with decompensated hydrocephalus.
MRI (Magnetic Resonance Imaging), like the CT scan, is a diagnostic technique that produces images of the brain—but unlike CT scanning, MRI does not use x-rays/radiation. Instead, MRI uses radio signals and a very powerful magnet to scan the patient’s body, and the signals are then formed into pictures by a computer. MRI is a painless procedure and has no known side effects.
There are two types of MRI scans:
- The Single Shot Fast Spin Echo (also called a “‘quick brain MRI”), which takes about three minutes and rarely requires sedation, is used to assess ventricular size.
- The full MRI, which takes 30 to 60 minutes and may require sedation for those prone to claustrophobia or anxiety, shows more minute details.
The radiologist will review the scans, write a report, and send the report on to the doctor.
It is sometimes necessary to perform an MRI with and without contrast enhancement. An MRI with the addition of a chemical agent enhances and improves the quality of the MRI image, allowing the doctor to look for subtle signs of tumor or chronic infection, which can cause adult-onset hydrocephalus and which may require additional treatment besides shunt surgery. Prior to the MRI, a doctor or technician will inject the dye agent either directly into your arm or through an IV. The MRI will then proceed as normal.
Neuropsychological Evaluation
A neuropsychological evaluation may also be recommended. The decision to order a particular test may depend on the specific clinical situation, as well as the preference and experience of the medical team.
Neuropsychology is about the studying how the brain and behavior are connected. When someone’s primary problems include thinking, emotion, and behavior, a neuropsychological evaluation can help doctors make a diagnosis. This evaluation can also help family members and doctors understand the effects of hydrocephalus on a person’s everyday life.
For neuropsychological assessments, a thorough interview is usually with the patient and sometimes one or more family members. The doctor also reviews the person’s medical records and test results. Following, a series of tests given to assess various parts of cognitive function, including attention, memory, language, visual-spatial ability, and executive function (the ability to reason, plan, and modulate behavior). The ultimate goal is to understand how changes in brain structure and function are affecting the patient’s behavior.
In the case of hydrocephalus in adults, neuropsychological testing can help serve as a tool to determine whether or not a patient would benefit from immediate surgical intervention or should simply be monitored for a longer period. Furthermore, the pattern of neuropsychologic impairment can help determine if a patient’s cognitive symptoms are consistent with hydrocephalus or are more likely due to another co-existing neurologic condition.
Additional Testing
More tests are often performed in adults to diagnose the condition. These tests may include:
- lumbar puncture
- continuous lumbar CSF drainage
- intracranial pressure (ICP) monitoring
- measurement of cerebrospinal fluid outflow resistance
- isotope cisternography
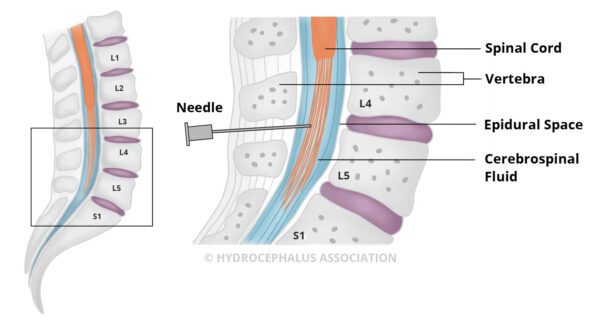 A lumbar puncture, also known as a spinal tap, allows an estimation of CSF pressure and analysis of the fluid. Under local anesthetic, a thin needle is passed into the spinal fluid space of the lower back. Up to 50 cc of CSF is removed to see if symptoms are temporarily relieved by this CSF volume reduction. If the removal of CSF dramatically improves symptoms, even temporarily, then surgical treatment is likely to be successful. The absence of improvement following a lumbar puncture, however, does not eliminate the possibility of improvement with shunt surgery. It is well-recognized that many patients who experience little or no improvement after the test may still improve with a shunt. It is helpful to have quantitative gait/cognitive testing before and after the LP to assess the significance of the degree of improvement.
A lumbar puncture, also known as a spinal tap, allows an estimation of CSF pressure and analysis of the fluid. Under local anesthetic, a thin needle is passed into the spinal fluid space of the lower back. Up to 50 cc of CSF is removed to see if symptoms are temporarily relieved by this CSF volume reduction. If the removal of CSF dramatically improves symptoms, even temporarily, then surgical treatment is likely to be successful. The absence of improvement following a lumbar puncture, however, does not eliminate the possibility of improvement with shunt surgery. It is well-recognized that many patients who experience little or no improvement after the test may still improve with a shunt. It is helpful to have quantitative gait/cognitive testing before and after the LP to assess the significance of the degree of improvement.
This test is extremely important if the cause of the hydrocephalus is not obvious. Occult infections or tumors with CSF spread may be found from culturing and analyzing the CSF for tuberculosis or fungi.
External lumbar drainage, also called lumbar catheter insertion or continuous lumbar drainage, is a variation of the lumbar puncture where a thin, flexible tube, called a catheter, is left in place to drain CSF. The procedure, which is performed in the hospital, allows for either intermittent or continuous removal of spinal fluid over several days to imitate the effect that a shunt would have. It also allows for a more accurate recording of CSF pressure. With an intermittent drainage protocol, the person is free to move around when the fluid is not being drained. Spinal fluid drainage over time can be thought of as a “test drive” of a shunt without actually undergoing shunt surgery. Patients who respond dramatically to such spinal fluid drainage are likely to respond to shunt surgery.
Nevertheless, a small proportion of patients who do not improve with lumbar drainage can still benefit from shunt surgery. However, because it requires hospitalization and has associated risks, it may not be recommended for all patients.
Intracranial Pressure Monitoring (ICP) is a diagnostic test that helps your doctors determine if the pressure in your head is too high or low and is causing your symptoms. To do this, ICP monitoring requires that you stay in the hospital. During the procedure, your surgeon will make a small hole in your skull, called a burrhole, and place a small pressure monitor into the brain or ventricles to measure the ICP. This monitor measures the pressure in your head directly using a small pressure-sensitive probe that is inserted through the skull.
Isotopic Cisternography, more involved than CT scan or MRI, is not widely used. Using the injection of tracers, it highlights the absorption of the CSF. It involves having a radioactive isotope injected into the lower back through a spinal tap, in order to monitor the absorption of CSF over a period of several days. This test is done in the hospital. This test is done in the hospital and has become less popular because a “positive” cisternogram result does not reliably predict whether a patient will respond to shunt surgery. Its utility in hydrocephalus in adults is not known.
NOTE: Not all of the tests listed are required in order to make a diagnosis.
At this point in the diagnostic process, it is important that a neurologist and a neurosurgeon become part of your medical team, along with your primary care physician. Their involvement from the diagnostic stage onward is helpful not only in interpreting test results and selecting likely candidates for treatment but also in discussing the actual surgery and follow-up care, as well as expectations of surgery.
How is Hydrocephalus Treated in Adults?
While there is currently no known way to prevent or cure hydrocephalus, there are three life-saving treatment options, all requiring brain surgery.
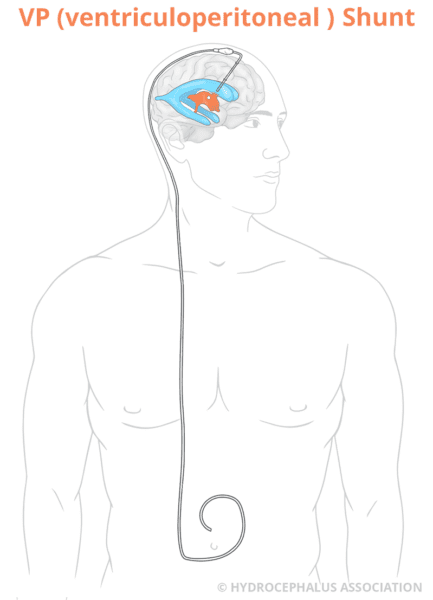
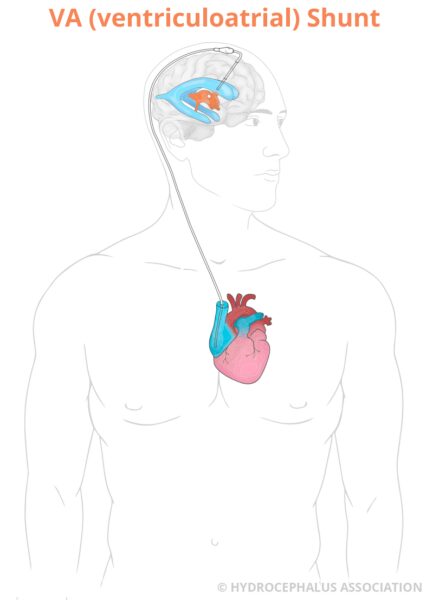
Shunt System

The most common treatment for hydrocephalus is a medical device called a shunt. The purpose of the shunt is to reduce the pressure inside the brain by draining the excess fluid, cerebrospinal fluid (CSF). The shunt diverts the fluid to another part of your body, most often the abdominal cavity or heart where it can be absorbed.
To learn more about a shunt, please visit our Shunt System page and What to Expect with Hydrocephalus Shunt Surgery page.
ETV (Endoscopic Third Ventriculostomy)
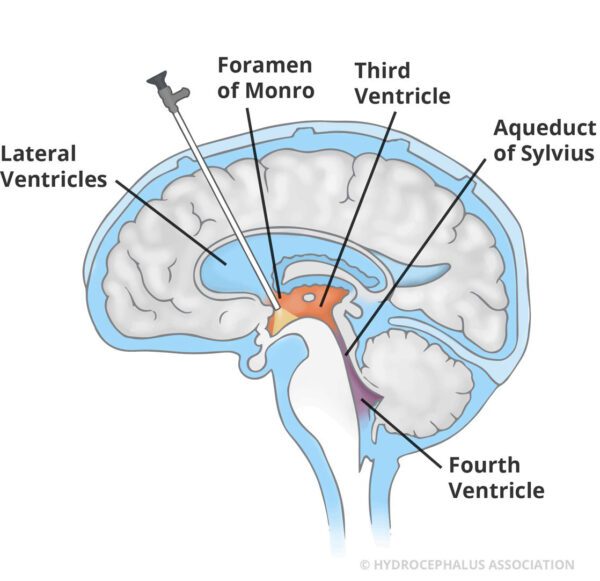
With this procedure, an endoscope (a small tube with a camera) is used to puncture a hole in the membrane on the floor of the third ventricle. This opens a natural pathway that allows CSF to flow out of the ventricles and around the brain, bypassing a blockage. An ETV is an important alternative to shunting for some cases of obstructive hydrocephalus and may be useful in other cases as well. This treatment option is not suitable for everyone and it is typically used for patients over the age of 2 who have a non-communicating (obstructive) hydrocephalus, but can be considered in other situations, as well. Non-communicating hydrocephalus occurs when there is a blockage within the ventricles of the brain, like aqueductal stenosis.
Endoscopic Third Ventriculostomy (ETV) with Choroid Plexus Cauterization (CPC)
This surgery, primarily performed in infants, involves the addition of choroid plexus cauterization (CPC) to the ETV. The choroid plexus is a network of vessels in the ventricles of the brain where cerebrospinal fluid is produced. Once inside the brain, the neurosurgeon uses a device to burn, or cauterize, choroid plexus tissue to reduce the amount of fluid being introduced into the ventricles. The fluid then passes through the opening made during the ETV and into the space surrounding the surface of the brain. This treatment is primarily used in children under the age of 2.
For additional information on ETV and ETV/CPC procedures, please explore our page dedicated to ETV and ETV with CPC, as well as our page detailing what you can anticipate during ETV surgery.
With early detection, effective treatment and appropriate interventional services, the outlook for adults with hydrocephalus is promising.
To find an adult neurosurgeon, visit our Physician Directory.
How is Hydrocephalus Managed in Adults?
Investments in research and advances in technology, as well as diagnostic and treatment protocols, are helping more and more people with hydrocephalus to lead full and active lives. But it is important to understand that life with a shunt or ETV does require you to always be well-informed and vigilant about complications. While some people can go 20 years or more without a complication, with a complex condition like hydrocephalus, things can change quickly therefore it’s critical to be prepared.
What are Possible Complications After Surgery for an Adult with Hydrocephalus?
When things are going well, it’s easy to put the concerns about hydrocephalus and the complications that come with it out of your mind. However, shunts can malfunction or become infected and this requires a shunt revision, which requires brain surgery. An ETV can close at any time and put an individual in an emergency situation.
Complications of a Shunt
Sometimes shunts can malfunction (fail) or become infected. Some of the signs and symptoms to watch for include:
- Headaches
- Nausea and/or vomiting
- Excessive tiredness
- Difficulty waking up or staying awake (this symptom requires urgent attention as it can potentially lead to a coma)
- Vision problems (such as double or blurred vision)
- Irritability (Changes in behavior or personality)
- Decline in job performance
- Loss of coordination or balance
- Difficulty concentrating or focusing
- Return of pre-treatment problems
- Fluid leaking from the shunt incision sites, potentially present with shunt failure or infection
- Signs of infection, such as fever, redness, or swelling at the shunt site
You may require a shunt revision, which requires another brain surgery. Please contact your healthcare provider right away.
Complications of an ETV
An ETV can close at any time and put an individual in an emergency situation. It is critical to understand the signs and symptoms of closure of an ETV. The symptoms are often similar to those of shunt failure. When an ETV fails it requires another brain surgery to reopen the hole.
See our page on ETV complications for a detailed list of signs and symptoms.
Seeking immediate medical attention can identify a resolvable complication and enable you or your family member to avoid brain damage or even death.
What is the Prognosis for Adults with Hydrocephalus?
In many cases, prompt treatment of hydrocephalus in adults can reverse many of the symptoms, restoring much cognitive and physical functioning. With proper management, many adults diagnosed with hydrocephalus lead full and fulfilling lives.
What can you expect?
Although hydrocephalus is a complex condition, the long-term effects can vary greatly from person to person. Prognosis depends on the cause, individual symptoms, the timeliness of diagnosis, and how well the person responds to the chosen treatment.
Potential Complications
Some general problems we see across our patient population include but are not limited to headaches, chronic pain, and psychosocial, emotional, and occupational issues. Coping with a condition like hydrocephalus can sometimes lead to emotional and psychological challenges. Feelings of uncertainty, stress, and anxiety can arise not only for individuals but also for their families as they navigate the complexities of the condition.
However, it’s important to know that timely diagnosis and effective treatment can significantly improve outcomes. If left untreated, progressive symptoms can become disabling, leading to severe cognitive and physical decline. Complications due to hydrocephalus can sometimes be fatal.
The length of time between the onset of symptoms and diagnosis is a factor in the success of treatment. Another, as yet unmeasurable, factor that affects the outcome of treatment is the extent of reversible versus irreversible brain injury caused by hydrocephalus. Treatment is most successful when little irreversible injury has occurred.
Remember, You’re Not Alone on This Journey.
Dealing with hydrocephalus can be challenging and unpredictable, but there is hope and support available. The Hydrocephalus Association provides essential tools and resources to empower you to regain control of your life.
The journey with hydrocephalus can be challenging and unpredictable. We provide essential tools and resources that enable you to have more control of your life.
There is a large community across the country that is engaged and connected through the Hydrocephalus Association ready to support you and your family. By staying well informed and planning appropriately, you or your loved one can realize their dreams of graduating college, pursuing and maintaining a career, getting married, having a family, and enjoying retirement.
For more detailed information, visit Daily Life.
Research and Hydrocephalus
As the leading private funder of hydrocephalus research in the country, we are investing in research to improve outcomes, prevent the development of hydrocephalus, and, ultimately, find a cure. The Adult Hydrocephalus Clinical Research Network (AHCRN) is a network of hospitals that conduct clinical research on hydrocephalus to improve treatment for the adult forms of hydrocephalus, including transitional patients who were diagnosed as children, those who acquire hydrocephalus as adults, and patients with normal pressure hydrocephalus.

You can be a part of the research. Enroll in HAPPIER, the only hydrocephalus patient-powered registry in the country, and help our doctors and scientists better serve you!
“Living with hydrocephalus has its challenges, but it’s taught me resilience and the importance of seeking support. With the right medical care, a strong support network, and determination, I’ve been able to overcome many obstacles and live a fulfilling life. There is hope in every step forward, and I believe that anyone facing hydrocephalus can find the strength to pursue their dreams and aspirations.” — Jennifer Bechard, living with Adult Hydrocephalus
Information you can trust! This article was produced by the Hydrocephalus Association, copyright 2024. We would like to thank James B. Golomb, MD for his valuable contribution and expert input.